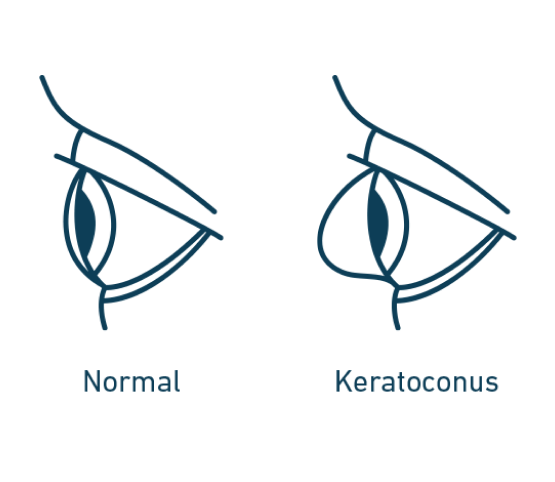
What is Keratoconus
Keratoconus, often referred to as "KC," is a non-inflammatory eye condition in which the typically round dome-shaped cornea progressively thins and weakens, causing the development of a cone-like bulge and optical irregularity of the cornea. This causes "static" in your vision and can result in significant visual impairment. KC can result in significant vision loss and may lead to a corneal transplant in severe cases.\The exact cause of KC is unknown, but genetics, the environment, and the endocrine system (which includes hormonal changes) could play a role in the development of KC. And, yes, excessive eye rubbing may contribute, too.
Keratoconus typically affects males and females alike, but some studies have shown a higher rate in males. The disease is also found in all ethnic groups with some studies showing higher incidence rates among Asian, black, and Hispanic populations.
Keratoconus Symptoms
Keratoconus may affect one eye at first but usually progresses to both eyes. Typical symptoms include:- Distorted vision
- Blurry vision
- Sensitivity to light
- Increased nearsightedness
- Symptoms can make day-to-day activities, such as driving or reading, difficult or impossible
- If left untreated, keratoconus can result in permanent vision loss.
Keratoconus typically first appears in individuals who are in their late teens or early twenties, and may progress for 10-20 years and then slow or stabilize. Each eye may be affected differently.
The cornea is responsible for focusing most of the light that comes into the eye. Therefore, abnormalities of the cornea, such as keratoconus, can have a major impact on how an individual sees the world, making simple tasks such as driving a car or reading a book very difficult.
iLink ™ Corneal Cross-Linking
iLink™ corneal cross-linking is a minimally invasive outpatient procedure that combines the use of ultraviolet light and specially formulated eye drops to stiffen and strengthen corneas that have been weakened by disease or refractive surgery. Cross-linking is considered the standard of care around the world for progressive keratoconus and corneal ectasia following refractive surgery.What is iLink ™ corneal cross-linking?
iLink ™ is the only FDA-approved corneal cross-linking procedure for the treatment of progressive keratoconus, which means it has been proven safe and effective in rigorous clinical studies. This minimally invasive outpatient procedure uses specially formulated prescription eye drops called Photrexa® (riboflavin 5'-phosphate ophthalmic solution) and Photrexa® Viscous (riboflavin 5'- phosphate in 20% dextran ophthalmic solution), combined with ultraviolet (UV) light from the KXL® System, to slow or halt the progression of diseaseWhat is Riboflavin?
Under the conditions used for iLink ™ corneal cross-linking, specially formulated pharmaceutical- strength riboflavin eye drops called Photrexa® and Photrexa® Viscous enable the cross- linking reaction to help slow or stop keratoconus from progressingWhat can I expect during the procedure?
- After numbing drops are applied, the epithelium (the thin layer on the surface of the cornea) is gently removed.
- Photrexa® Viscous eye drops will be applied to the cornea for at least 30 minutes
- Depending on the thickness of your cornea, Photrexa® drops may also be required
- The cornea is then exposed to UV light for 30 minutes while additional Photrexa® Viscous drops are applied
What can I expect after the procedure?
- You should not rub your eyes for the first 5 days after the procedure
- You may notice a sensitivity to light and an uncomfortable sensation in the treated eye. Sunglasses may help with light sensitivity
- If you experience severe pain in the eye or any sudden decrease in vision, you should contact your physician immediately
- If your bandage contact lens from the day of treatment falls out or becomes dislodged, you should not replace it. Contact your physician immediately


