Blocked Tear Ducts in Children
 Blocked tear ducts are a fairly common problem in children. It has been estimated that approximately 5% of babies have tear duct problems. Although the vast majority of them get better on their own, not all do. In order to best understand how a blocked tear duct is treated, it helps to know something about the way a normal tear duct functions.
Blocked tear ducts are a fairly common problem in children. It has been estimated that approximately 5% of babies have tear duct problems. Although the vast majority of them get better on their own, not all do. In order to best understand how a blocked tear duct is treated, it helps to know something about the way a normal tear duct functions.
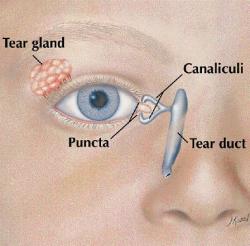
Normal Anatomy: Tears are normally made in the tear gland, which is under the upper eyelid near its outer (lateral) corner. You can see it in the drawing below. Tears are continuously secreted by this gland and lubricate the eye to keep it moist. At the same time, tears are draining away from the eye through two holes, one on the upper and one on the lower eyelid. These holes are called the puncta and are openings to the tear drainage system. Look for the location of the puncta in figure A. If you look closely at your own eyelids in a mirror, or those of your child, you should be able to see these pinpoint sized openings on the edge of the eyelids in toward the nose. After passing through the puncta, tears flow through a canal in the upper and lower eyelid called the canaliculi. These canaliculi then join together and empty into a larger sack, which is in fact called the lacrimal (or tear) sac. Tears then exit through the bottom of the tear sac to drain through another duct-the nasolacrimal (or tear) duct which goes through the bone into the nose. That is why your nose runs when you cry! These structures, the canaliculi, lacrimal sac, and nasolacrimal duct, are all under the skin and are not visible to the naked eye. The figure below helps to show where they are located.
Blocked Tear Ducts: When a baby is developing, before they are born, there is normally a membrane blocking the opening of the tear duct into the nose. Around the time a child is born, this membrane opens up. Failure of this membrane to open is the most common cause-but not the only cause- of a blocked tear duct. This may happen in one or both eyes. If the tear duct is blocked, tears may still enter the upper part of the tear drainage system (the puncta, canaliculi, and tear sac); however, they cannot drain all the way into the nose because of the blockage. Think of this like a sink in which the water is running, but the drain is plugged. In the case of a sink, the water will overflow. In the case of a blocked tear duct, the eye is constantly watering and the tears drain down the child's cheek. Also, mattering (pus-like drainage or crusting of the eyes) is a common symptom in children with blocked tear ducts. Just as stagnant water in a pond breeds bacteria, the tears that are trapped in the tear sac get infected. This shows up as pus-like drainage from the eyes. Often the eyelids are mattered and stuck shut in the morning. Often parents are surprised to hear their child's tear ducts are blocked, when the child's eyes are always watery. Once one understands it is not the duct from the gland that produces tears that is blocked, but rather the duct that normally drains tears away from the eye, this apparent contradiction is less confusing. Even though the blockage of the tear ducts is present at birth, there commonly are no symptoms until a child is several months old. This is because newborn's tear gland does not produce as much liquid as it does when the child is a bit older. The symptoms of blockage of the tear duct do not appear until there is more tear production.
Treatment of Blocked Tear Ducts: It has been estimated that about 85% of children with blocked tear ducts get better on their own. Initially, treatment is aimed at keeping the mattering (infection) from getting out of hand, and encouraging the natural process of the blockage opening up. In very mild cases, nothing may need to be done while you are waiting for healing. If there is much mattering of the eye(s), antibiotics in the form of eye drops or ophthalmic ointment may be prescribed. This usually has a dramatic effect on quieting down the mattering. However, antibiotics will not do anything to actually cause the tear duct to open. Their use merely allows us to bide time while we are waiting for nature to cure the problem. For this reason, parents of babies with blocked tear ducts often report that their baby seems cured while on antibiotic eye drops. However, the problem recurs as soon as the medication is stopped. In many cases, massaging the tear duct in a specific way may result in the tear duct opening. You should place your thumb or forefinger on the skin just above the tear sac. Then, with a rather firm movement, you should stroke downward. The idea is to get some of the pus or fluid that is in the tear sac trapped between your finger and the membrane that is blocking the tear duct. With firm downward pressure, the pus or fluid may be squeezed downward and rupture the membrane. If that occurs, the symptoms of a blocked tear duct suddenly improves. It would be more accurate if this maneuver was called "milking" the tear duct, rather than "massage." Generally, it is recommended that parents do this for about 5-10 strokes, 3 or 4 times a day for several weeks.
Probing of a Tear Duct: If a blocked tear duct does not improve, probing of the tear duct is the recommended method of treatment. This involves passing a thin wire probe into the puncta and down the tear duct to open the membrane. If the tear duct is blocked because of the mechanism described above (a membrane at the bottom of the tear sac) probing is successful in about 95% of cases. In a small number of children, a more involved procedure as described below may be necessary. Also, sometimes the tear duct system has a more complicated type of obstruction. There may be multiple kinks of strictures in the canaliculi, or on occasion, the entire tear duct system may have not developed properly. Your ophthalmologist can tell if this is the case at the case at the time of probing. If a more complex type of obstruction is found, simple probing may not be curative. In this situation, one of the more involved procedures described below may be needed.
When a Tear Duct Should Be Probed: As stated above, about 85% of all children with blocked tear ducts get better without needing probing. However, most children improve on their own in the first month of life, the next most in the second, and so on. By the time a child is 6 months old, there is still a small likelihood he will get better. However, the odds are less than they were at birth. Most (but not all) children who are destined to improve do so by one year of age.
What You Should Expect if Your Child Has a Tear Duct Probing: Immediately after a tear duct probing, there may be mild bloody drainage from the nose and/or the eye for several hours; this is normal. You may be given an eye medication (drops or ointment) to put in the eye(s) several times a day for a week or so after the probing. There are no limitations on activity after the procedure is completed.
If Tear Duct Probing is Not Successful: In the vast majority of cases, a simple tear duct probing is successful in curing the problem of a blocked duct. For those children where probing is not successful, there are several alternative treatment options. One option is to repeat the probing, and insert a silicone tube in the tear duct. Leaving the silicone tube in place for a number of months may prevent the tear duct from scaring closed. This option is particularly helpful when the blockage is in the upper part of the tear duct system. Another option is to repeat the probing with a special probe that has a balloon at the end, which can be inflated in the tear duct to stretch it open. This procedure is similar to the angioplasty procedure that is done to open blocked arteries in the heart. Finally, and infrequently, an actual surgical procedure may be needed to make a completely new drainage opening for the tear duct system.
Conclusion Although blocked tear ducts represent a very common problem, they can almost always can be completely corrected.
(Adapted from information prepared by the Public Information Committee of the American Association for Pediatric Ophthalmology and Strabismus)

